Herniated Disc

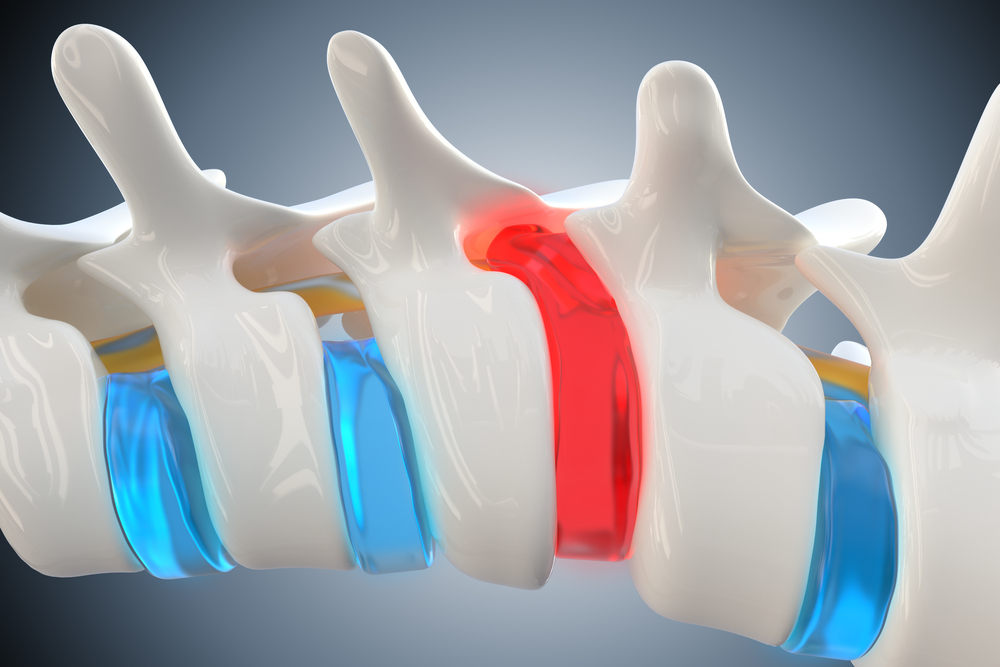
Cervical herniated disc is a condition that occurs when the outer layer of a disc in the neck region tears, causing the inner material to protrude and potentially irritate nearby nerves. This condition can lead to symptoms such as neck pain, radiating pain into the arms or shoulders, numbness or tingling along affected nerve pathways, muscle weakness, and, in some cases, headaches. Causes of cervical herniated discs include wear and tear, aging, and injury. Factors such as repetitive motion, poor posture, and sudden trauma can contribute to the development of herniations. The aging process can also lead to disc degeneration, making the discs more susceptible to herniation. Diagnosis involves a thorough examination by healthcare professionals and often includes imaging tests such as MRI or CT scans to determine the location and severity of the herniation. Treatment options for cervical herniated discs typically begin with conservative measures, including rest, medication (pain relievers and anti-inflammatories), physical therapy with strengthening exercises and stretches, and heat/cold therapy to alleviate discomfort. If symptoms persist or worsen, surgical intervention may be considered. Procedures like discectomy or cervical fusion aim to alleviate pressure on the nerves and restore spinal stability.




Book an appointment
"*" indicates required fields